Many of my patients are surprised when I recommend a gut repair and restore protocol as part of their personalized treatment plan.
“What does my gut have to do with my sinus allergies?” they ask, or “How will repairing and restoring my gut improve my mood and energy?” These are fair questions. The link between the gut and certain illnesses is counterintuitive — at least on the surface.
But that should come as no surprise. Since the earliest days of medicine, physicians have recognized the importance of gut health and function on overall health. In fact, Greek physician Hippocrates, widely considered the father of Western medicine, claimed that “all disease starts in the gut.”
In this two-part series, I explore the vital role that the gastrointestinal system (the gut) plays in overall health, symptoms that frequently accompany gastrointestinal dysfunction, and the four-step protocol I often use with patients to restore and optimize gut health and function.
How the Gut Supports Overall Health
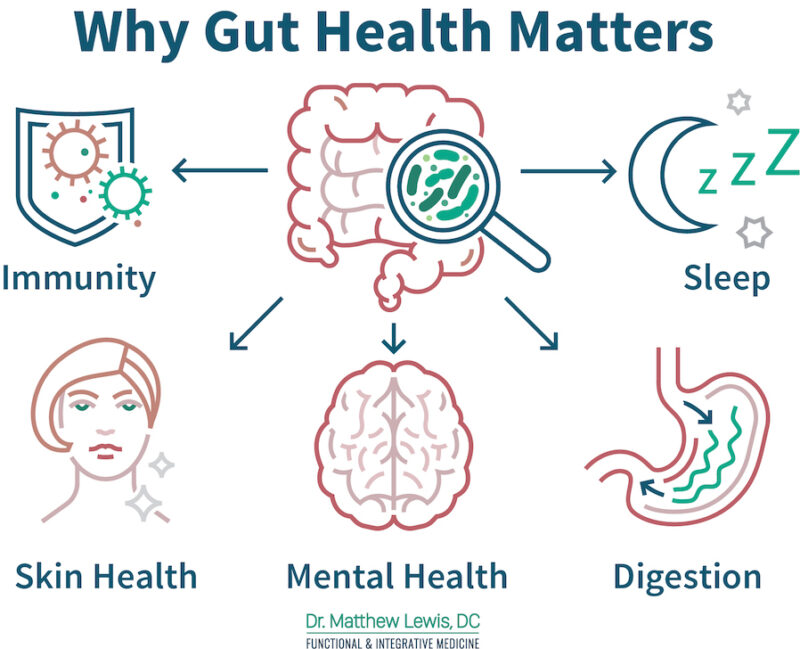
Although I wouldn’t go so far as to say all disease starts in the gut, the gut does have a positive impact on health in many ways, including the following:
- Enables digestion and nutrient absorption. Breaks down food into nutrients such as carbohydrates, proteins, fats, vitamins, and minerals, which can then be absorbed and transported through the bloodstream to various parts of the body.
- Prevents infection. According to some estimates, the gut makes up nearly 70 percent of the body’s immune system. The gut helps defend against infectious agents (bacteria, virus, fungi, and parasites) in many ways, starting with stomach acid, which eradicates many potential pathogens in food on contact. Additionally, gut-associated lymphoid tissue (GALT) helps monitor and defend against pathogens and other foreign substances. And microorganisms living in the gut play a key role in the formation of T cells (white blood cells that play a major role in the adaptive immune response).
- Provides an environment for beneficial microorganisms. A diverse community of microorganisms living in the gut plays a vital role in digestion, nutrient synthesis and absorption, immune function, and mood regulation.
- Assists in regulating metabolism. Microorganisms living in the gut influence how the body extracts energy from food and regulates metabolism. Imbalances in the community of microorganisms have been linked to conditions such as obesity and metabolic disorders.
- Synthesizes essential nutrients. Certain microorganisms living in the gut are responsible for synthesizing chemical compounds that are essential for the body to function, but that are not present in sufficient quantities in the food we eat.
- Supports neurological health. The gut and brain communicate with one another through various pathways to ensure proper function of both. This communication also influences mood, behavior, and cognitive function.
- Helps regulate inflammation. A healthy gut allows nutrients to pass through it into the bloodstream while preventing the passage of pathogens (such as bacteria and viruses) and small molecules from foods that can trigger an immune response. When the gut lining is damaged, substances that should be contained within the gut escape into the bloodstream and may trigger an immune response. That can result in inflammation and over time, the development of autoimmune conditions.
- Helps eliminate waste. The muscular walls of the gut relax and contract to move waste products through the digestive tract — an action known as motility. Proper motility prevents constipation and diarrhea and helps to remove toxins and other harmful substances from the body.
- Assists in hormone regulation. The gut communicates with the body’s endocrine system to help regulate the production and release of hormones that impact appetite, satiety, blood sugar levels, and other bodily functions.
Factors That Can Negatively Impact Gut Health
Many factors can negatively impact gut health, including the following:
- Antibiotics, which can kill beneficial microorganisms as well as harmful ones
- Medications for reducing stomach acid — the body’s first line of defense against disease-causing bacteria, fungi, viruses, and parasites in food
- Poor diet (for example, high in sugars and other simple carbohydrates and low in healthy proteins, health fats, and fiber)
- Brain trauma or other brain or nervous system disorders that affect motility — the movement of food and waste through the digestive tract
- Lack of physical activity, which can also negatively impact motility
- Traumatic or chronic stress
- Bacterial or viral infections, some of which can trigger inflammatory responses that damage the lining of the gut, making it more permeable
- Birth by cesarean section, which may limit a newborn’s exposure to beneficial microorganisms present in the birth canal, preventing them from colonizing the infant’s gut
- Toxic or unhealthy substances, such as alcohol, nicotine, environmental toxins, medications, and illicit drugs, which can cause imbalances
Typically, gut health is compromised not by a single cause, but by a cluster or series of events. For example, a patient sees her doctor for a bacterial infection. The doctor prescribes an antibiotic, which cures the infection but causes a microbial imbalance in the gut that leads to an overgrowth of candida yeast. The yeast damages the intestinal lining, allowing allergens to enter the bloodstream, triggering an immune response that causes an inflammatory bowel condition. By the time the patient reports symptoms of that condition, several health issues need to be addressed — candid yeast overgrowth, inflammation, immune dysregulation, damage to the intestinal lining, and the initial microbial balance.
Obvious and Not So Obvious Digestive Symptoms
Many patients have symptoms clearly indicative of compromised gut health, such as the following:
- Bloat: Distended or stretched belly, feeling full and uncomfortable even after having little or nothing to eat
- Heartburn: A burning sensation in your chest (sometimes worse at night), chest pain, difficulty swallowing, regurgitation of food or sour liquid, the sensation of having a lump in your throat, chronic cough, laryngitis, new or worsening asthma, poor sleep — these symptoms may lead to a diagnosis of gastroesophageal reflux disease (GERD) or acid reflux
- Diarrhea: Loose, watery, and possibly more frequent bowel movements
- Irritable Bowel Syndrome (IBS): Diarrhea, constipation, alternating diarrhea and constipation, abdominal discomfort related to bowel movements, mucus in stool, urgency, or feeling of incomplete evacuation
- Colitis (literally inflammation of the colon): Abdominal cramps, abdominal pain, mucus, blood in the stool (dark stools the consistency of tar), diarrhea, bloating, chills, dehydration, fatigue, fever, joint pain, weight loss, vomiting
- Constipation: Fewer than three bowel movements a week, hard or lumpy stools, straining to have a bowel movement, feeling as though you have a blockage preventing a bowel movement, feeling as though you cannot completely empty your bowel
For many patients, their gastrointestinal issues produce symptoms that you would never imagine are related to gastrointestinal damage or dysfunction, such as the following:
- Migraines
- Aches and pains
- Fatigue
- Food allergies or intolerances
- Brain fog (difficulty concentrating)
- Mood irregularities (depression, anxiety)
- Skin issues, such as acne, eczema, or rosacea
- Hormonal imbalances (irregular periods or PMS)
- Seasonal allergies (runny nose, sinus congestion)
- Autoimmunity (rheumatoid arthritis, Hashimoto’s thyroiditis, lupus, psoriasis, or celiac disease)
- Chronic fatigue
- Fibromyalgia
In many cases, patients with compromised gut health consult with many doctors and specialists who order numerous lab tests that all come back normal. They conclude that nothing is medically wrong, or they merely treat the symptoms and never even suspect a problem with the gut or digestion.
The good news is that a functional medicine approach to healthcare offers testing to diagnose or rule out digestive dysfunction and an effective treatment protocol for restoring and optimizing gut health and function. Check in next week for the second installment in this series, “Restoring Gastrointestinal Health and Function: Part Two — Testing and Treatment.”
In the meantime, if you’re concerned about any of the issues outlined above and would like to meet with me to discuss your health, please reach out. The best way to connect with me about an initial consultation is by using the Contact Form here on my website.
– – – – – –
About the Author: Dr. Matt Lewis, D.C., DACBN, CFMP®, specializes in diagnosing and treating the underlying causes of the symptoms related to chronic and unexplained illness through nutrition, lifestyle, chiropractic, and other natural approaches to whole-health healing in Tampa, Fla. Dr. Lewis has 20 years of experience practicing nutritional and holistic medicine. He earned his B.S. in Biology from Shenandoah University, his Doctorate in Chiropractic from Life University, his Diplomate status in Clinical Nutrition from the American Clinical Board of Nutrition, his CFMP from Functional Medicine University, and his certification as a Digestive Health Specialist (DHS) through the Food Enzyme Institute. Dr. Lewis’ passion for health and wellness stems from his own personal experience. With a family history of autoimmune conditions and diabetes, and his own lab tests showing his genetic susceptibility to Hashimoto’s thyroiditis (autoimmune thyroid), Dr. Lewis has learned how to restore his own health and vigor to prevent the onset of these and other illnesses and live an incredibly active life. Through this process, he acquired a deeper understanding of health and wellness, which he now offers his patients in Tampa and elsewhere.



Leave A Comment