Benefits of Boosting Human Growth Hormone (HGH) for Recovery and Resilience
For many of us, as children and teenagers and even into our 30s, we found ourselves strong and energetic, recovering quickly after moderate and even intense exercise, and often immune to daily aches and pains. As we aged beyond those years, however, we started to lose our stamina and ability to quickly recover.
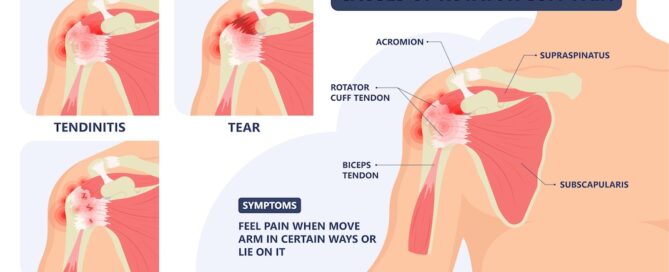
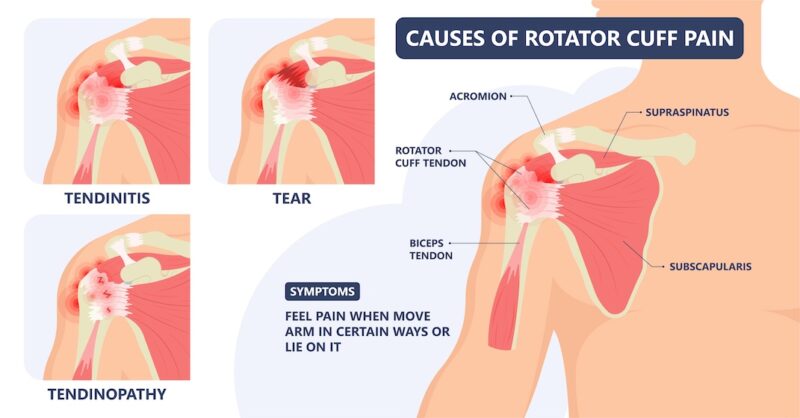
More and more exercise is required just to maintain our strength, flexibility, and vitality. It takes longer for us to recover from those exercise sessions, and we’re more susceptible to injury. Why is this? What do we lack in our later years that we had in abundance in our youth?

The answer is human growth hormone (HGH). HGH stimulates and regulates the growth and lifecycle of nearly every cell in the body. And when you reach the age of about 30 years, your pituitary gland releases less and less HGH with each passing year. This decline can occur rapidly, and to be clear, it is a normal part of aging. However, this reduction of HGH is largely responsible for many of the signs associated with aging:
- Lower energy
- Decreased muscle mass and inability to build new muscle
- Increased difficulty losing or maintaining weight
- Weakened immune system
- Decreased healing efficiency
- Other signs of physical and mental aging
Today, I want you to know that by working with functional medicine-focused doctor, you can work on reversing this process and boost HGH in two ways:
- Directly via injections of synthetic human growth hormone, which is typically recommended only for people whose pituitary gland is damaged or dysfunctional
- Indirectly by stimulating the pituitary gland to release more human growth hormone that your body produces naturally
Stimulating the Pituitary Gland to Release More HGH Naturally
Stimulating the pituitary gland to release more human growth hormone is the safer way to increase HGH, and there are several ways to do it: Continue reading…